Use of 3D-planning and tantalum in revision total hip arthroplasty after failed iliac bone allograft for Ewing sarcoma: a case report
Introduction
Ewing sarcoma (ES) is the second most frequent malignant bone tumor in children (1). Pelvic ES, representing about 25% of cases, has presented poorer outcomes, because of delay in diagnosis, proximity to noble structures, and lack of anatomic barriers to tumor spread.
Current treatment for localized ES is a combination of chemotherapy, surgery and/or radiotherapy (RT). Surgery consists in a wide margins tumor resection and limb-preserving pelvic reconstruction.
Pelvic resections are classified by region: type I iliac, type II acetabular, and type III pubic. But in children, physeal cartilage may represent an oncologic barrier, providing an adequate margin for resection, while maintaining some part of the native acetabulum for use in the reconstruction.
The choice of the type of pelvic reconstruction after RT and resection with pelvic discontinuity and involving the acetabulum is complex. Massive grafts or custom-made pelvic prostheses can be used. However, the risk of complications is high, and it is increased by RT. In particular, RT complicates the consolidation of massive bone grafts and the retention of custom-made bulky implants. Moreover, the risk of infection is increased by the high amount of metal and RT. As a consequence, if revision surgery is required, the cause of the failure of the primary reconstruction must be carefully considered, particularly after infection.
With this report we describes a case of pelvic reconstruction with total hip arthroplasty (THA) revision components after failed iliac bone allograft for infection, following RT and a type I+II pelvic resection in a child with a Pelvic ES of the left iliac wing extended to the acetabular roof.
The first topic of this report is the role of 3D-printed pelvic model used to test matching degree of implant. The present case shows the application of preoperative simulation tools based on a 3D virtual model and of intra-operative use of a life-size physical model.
The second topic is the choice of the implant. Tantalum lead to a great osteointegration thanks to its high coefficient of friction (0.88) and porosity (80%) (2). The use of tantalum implants on irradiated bone in oncologic patients, has been reported with good results (3-5). We used a revision cup associated only with a straight buttress to perform hemipelvis reconstruction. This original combination restores the sacral-pelvis continuity, simplifies the procedure, minimizes the amount of metal implanted reducing the risk of infection, without sacrifices the implant stability.
We present the following article in accordance with the CARE reporting checklist (available athttp://dx.doi.org/10.21037/pcm-20-42).
Statement of informed consent
The patient and his parents were fully informed that data concerning his case would be submitted for publication. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient.
Case presentation
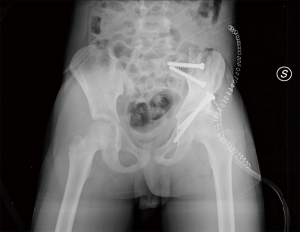
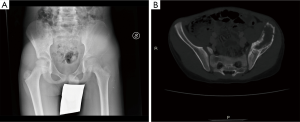
In March 2011, a 10-year-old patient presented with left ileo-inguinal pain, appearing one month before after sports activity. Remote pathological history was negative. X-ray and CT scan of the pelvis revealed a large area of osteolysis involving the left iliac wing and extended to the acetabular roof (Figure 1A,B), appearing extra-compartmental in at least two points (medium gluteus and ileo-psoas muscles). PET was positive in pelvis, chest CT scan negative for pulmonary localizations. Open biopsy confirmed the diagnosis of Ewing’s sarcoma, stage IIB according to Enneking. Neoadjuvant chemotherapy was started, according to ISG-AIEOP EW1 protocol. After 4 cycles, the volumetric reduction of the lesion was not satisfactory. Consequently, RT was associated, resulting in a negative PET in the pelvis. MRI showed that the lesion now appeared intra-compartmental and non-invasive to tri-radiated cartilage.
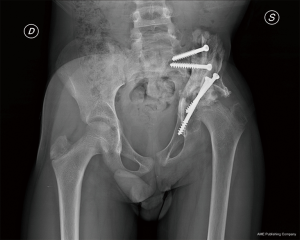
In May 2012, through skin incision following the iliac crest, the musculature was dissected off the pelvis to expose the ilium and acetabulum. Under fluoroscopic guidance, the triradiate cartilage was divided using an osteotome. The ilium superior to the triradiate cartilage was removed en bloc, with a part of the superior aspect of the acetabulum. An iliac bone allograft was placed in order to restore the anatomical congruence of the pelvis (Figure 2). Following a pelvic-podal plaster was packaged. The histological examination confirmed the wide margins of the resection, showing a 100% necrosis rate after neoadjuvant treatments. There was a residual dysmetria in minus on the left limb of 5 cm. At follow-up, no signs of local recurrence, but early signs of graft resorption (Figure 3).
In November 2014, a sacral screw protrusion and adjacent fistula were observed and surgically treated, diagnosing a Staphylococcus aureus graft infection.
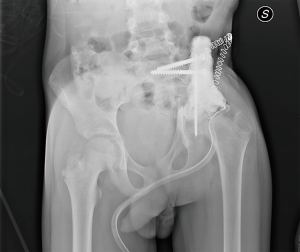
In February 2015, after pre-operative antibiotic-therapy with oxacillin, the graft was removed, and an antibiotic-laden cement spacer was placed (Figure 4). During surgery, a severe deterioration of the femoral head was confirmed. It followed antibiotic-therapy with cotrimoxazole and rifampicin, with inflammation relief.
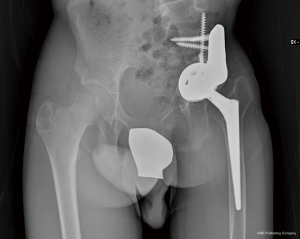
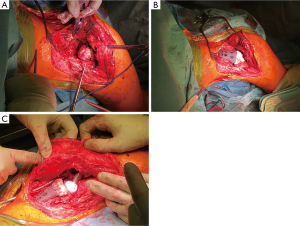
In February 2018, PET scan and laboratory analysis confirmed no residual infection. MRI shown no local recurrences. Therefore, the definitive reconstruction of the hemipelvis and THA were indicated and performed at the end of the growth, in March 2018. Due to the massive bone loss, in order to optimize the implant size and placement, a reconstruction planning using a virtual and physical 3D-model, based on high-resolution CT scan, was performed (Figure 5A,B,C). For the reconstruction (Figure 6A,B,C), a primary trabecular tantalum cup for THA (Continuum Acetabular Shells Trabecular Metal™ Multi-Hole, Zimmer Biomet) was implanted on the residual native acetabulum. A straight tantalum buttress (Straight Buttress Augment, Zimmer Biomet, Warsaw, Indiana, U.S.), usually used to reinforce acetabular roof, was associated as a bridge between cup and sacrum, reconstituting the continuity of the pelvic ring. The bone continuity was reconstituted by autologous grafts resulting from the femoral head, after extemporaneous histological examination which confirmed no sign of acute phlogosis. Actually, we believe that the use of autologous bone, even if irradiated, is preferable to allografts. The CT-based patient-specific printed 3D-model of the pelvis was useful to facilitate the planned placement of the implant components, providing anatomical landmarks. Then, the cup was fixed with two sacral screws and one screw through posterior acetabular wall. Three cancellous screws were used to fix the buttress to the sacrum. The cup and buttress were merged with cement. A conus stem (Wagner Cone Prosthesis®, Zimmer Biomet, Warsaw, Indiana, U.S.) was used to maximize diaphyseal fill and fit, due to the morphology of the proximal femur (Figure 7). Postoperatively, pelvic-podal plaster was packed for one month, followed by hip brace for 15 days. Afterwards, an incremental load was granted.

In March 2020, at last follow-up at 24 months to surgery, the CT artifacts caused by the implant do not allow to confirm the bone-union of the graft, but the implant is well-placed without signs of infection or recurrences. Clinically, the MSTS functional score was 70%, with good patient’s satisfaction, no pain, flexion up to 90° and good degree of rotations granted. Residual dysmetria of 9 cm will be corrected next by lengthening the femur with an expandable intramedullary nail.
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and national research committees and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
Discussion
The use of allografts of the pelvic bone is a well-known method of reconstruction after pelvic resection. However, reported complication rates have been 29% to 60% (6). Deep infection is the most frequent one (12% to 36%) and is a common cause of implant failure.
Preoperative RT increases histological necrosis of the resected specimens (6), but may contribute to increase the infection risk, as happened in our case. Campanacci et al. reported infection in 15% of patients after massive allograft reconstruction (7). However, functional results have often been good (8, 9), with better results in patients below 20 years (8). In our opinion, this evidence justifies the choice of the initial treatment in the case described above.
In type I ES, the possibility of preserving the acetabulum allows better functional result. The triradiate cartilage, acting as a barrier against the tumor spread, in some cases, may offer this strategy also for ES of the ilium extended to the acetabulum (type I+II). Preserving a part of the acetabulum may optimize reconstruction and outcome. Few kinds of reconstruction strategies are suitable after a type I+II resection, especially after previous procedures, as in our case, because the poor bone stock may provide not enough anchorages for the implant. To treat similar cases, Guo et al. reported the use of a pedicle screw-rod system augmented with cement in combination with an acetabular reinforcement shell and hip arthroplasty (10). We think that the method used in this report may easily restore the sacral-pelvis continuity and the function of the hip, maintaining optimal mechanical stability.
In recent years, 3D technology had been applied in orthopedic oncology with the production of protheses, osteotomy guides, and virtual or printed models. Although the use of 3D is a technically demanding process, requiring additional radiation exposure, advantages are well documented, especially for custom-made prosthesis, but we assume also for the use of 3D virtual and printed models. 3D-models may facilitate the preoperative planning and an accurate reconstruction of the joint, reducing operation time and intraoperative complications.
About the implant, tantalum has shown its effectiveness in revision THA, but there is limited evidence of its use in oncologic patients undergoing previous RT. Previous studies had shown how RT can affect both cemented and uncemented acetabular components, leading to aseptic loosening (5). Recently, the use of tantalum implants on irradiated bone, has been reported with good results in treatment of non-musculoskeletal tumors (3, 4). Instead, senior author of this report (MDP), using tantalum cups, reported an implant survival rate of 92% with a mean 68 months follow up, in patients with primary or secondary pelvis musculoskeletal tumors undergoing acetabular irradiation (5).
The main strength of the presented technique lies in its potential high reproducibility. The main limits are represented by the alteration of the hip rotation center and the restricted follow-up. This is the first case treated with this construct; larger series will be necessary to better define the reliability of this technique.
This report provides an interesting example of how the use of technological innovations, in this case represented by new informatics tools and new materials, can improve the clinical results of particularly demanding surgical procedures. We therefore suggest the evaluation of 3D-planning and tantalum in complex oncological reconstructions of the pelvis.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the CARE reporting checklist. Available at http://dx.doi.org/10.21037/pcm-20-42
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/pcm-20-42). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Jackson TM, Bittman M, Granowetter L. Pediatric Malignant Bone Tumors: A Review and Update on Current Challenges, and Emerging Drug Targets. Curr Probl Pediatr Adolesc Health Care 2016;46:213-28. [Crossref] [PubMed]
- Levine BR, Sporer S, Poggie RA, et al. Experimental and clinical performance of porous tantalum in orthopedic surgery. Biomaterials 2006;27:4671-81. [Crossref] [PubMed]
- Rose PS, Halasy M, Trousdale RT, et al. Preliminary results of tantalum acetabular components for THA after pelvic radiation. Clin Orthop Relat Res 2006;195-8. [Crossref] [PubMed]
- Joglekar SB, Rose PS, Lewallen DG, et al. Tantalum acetabular cups provide secure fixation in THA after pelvic irradiation at minimum 5-year followup. Clin Orthop Relat Res 2012;470:3041-7. [Crossref] [PubMed]
- De Paolis M, Zucchini R, Romagnoli C, et al. Middle term results of tantalum acetabular cups in total hip arthroplasty following pelvic irradiation. Acta Orthop Traumatol Turc 2019;53:165-9. [Crossref] [PubMed]
- Fujiwara T, Lex JR, Stevenson JD, et al. Surgical treatment for pelvic Ewing sarcoma: What is a safe and functional acetabular reconstruction when combined with modern multidisciplinary treatments? J Surg Oncol 2019;120:985-93. [Crossref] [PubMed]
- Campanacci D, Chacon S, Mondanelli N, et al. Pelvic massive allograft reconstruction after bone tumour resection. Int Orthop 2012;36:2529-36. [Crossref] [PubMed]
- Delloye C, Banse X, Brichard B, et al. Pelvic reconstruction with a structural pelvic allograft after resection of a malignant bone tumor. J Bone Joint Surg Am 2007;89:579-87. [Crossref] [PubMed]
- Hillmann A, Hoffmann C, Gosheger G, et al. Tumors of the pelvis: complications after reconstruction. Arch Orthop Trauma Surg 2003;123:340-4. [Crossref] [PubMed]
- Guo Z, Li J, Pei GX, et al. Pelvic reconstruction with a combined hemipelvic prostheses after resection of primary malignant tumor. Surg Oncol 2010;19:95-105. [Crossref] [PubMed]
Cite this article as: Fiore M, Sambri A, Zucchini R, Giannini C, Taddei F, De Paolis M. Use of 3D-planning and tantalum in revision total hip arthroplasty after failed iliac bone allograft for Ewing sarcoma: a case report. Precis Cancer Med 2020;3:30.