非小细胞肺癌免疫检查点抑制剂耐药后的治疗选择
简介
对于驱动基因阴性的非小细胞肺癌(NSCLC),免疫检查点抑制剂已逐渐走向一线治疗。对于PD-L1者,例如肿瘤比例评分(TPS)大于或等于50%者,帕博利珠单抗单药治疗在毒性反应、无进展生存期和总生存期上均优于双药化疗[1,2]。有关PD-L1表达的所有宣传中,非鳞NSCLC的帕博利珠单抗联合培美曲塞和顺铂/卡铂均优于单纯化疗[3]。阿特珠单抗联合多西紫杉醇,卡铂和贝伐珠单抗也优于三药方案[4]。在鳞癌中,阿特珠单抗联合卡铂和白蛋白紫杉醇提高了PFS和OS[5]。帕博利珠单抗联合紫杉醇或白蛋白紫杉醇和卡铂也获得了同样的疗效[6]。在高突变负荷的NSCLC中,无论PD-L1的表达情况如何,PD-1抑制剂和CTL4抑制剂的联合治疗获益均优于化疗[7]。此外,在同步放化疗后序贯度伐利尤单抗的强化治疗显示相应的生存优势[8,9]。充分的证据证明在一线化疗后PD-1和PD-L1抑制剂有效[10-13],然而几乎没有前瞻性数据为一线使用免疫检查点抑制剂后肿瘤复发和进展后续治疗提供依据。因此根据不同的一线治疗情况,以下我们将阐述一线免疫检查点抑制剂治疗后如何治疗的策略。当然,上述方案有待在未来通过注册的临床试验数据进行证实。
因毒性反应停止免疫检查点治疗后或者经长程治疗后出现疾病进展
若因毒性反应停止免疫检查点抑制剂治疗,其后出现进展,重新启用免疫检查点抑制剂不失为选择[14]。长期使用免疫检查点抑制剂治疗并获得持久的疗效,进展时再次引入免疫检查点抑制剂具备合理性[15]。该议题将在本期PCM的另一篇文章中阐述。
PD-1抑制剂单药治疗期间出现疾病进展
在PD-1抑制剂单药治疗过程中若出现疾病进展,可予以经典的双药化疗方案[3],且治疗强度合适。如果是单一/寡病灶进展,可添加局部治疗,特别是放射治疗[16,17]。放射治疗会产生免疫效应,可能导致照射区域外远处的肿瘤消退(远隔效应)[18]。一篇系统综述包含了从1969年到2014年共46个病例,在不同病种的各种不同临床情况下均可观察到远隔效应,最晚可在放疗后12个月出现[19]。远隔效应也可出现于放疗联合伊匹单抗治疗后[20]。在一项Ⅱ期临床试验中,寡转移局部消融治疗后予以帕博利珠单抗获得了良好的PFS和OS[21]。放疗和其他免疫治疗的联合也可作为临床试验中的选择[22,23]。获得性耐药的原因包括T细胞耗竭,可以通过增加旁路刺激克服上述问题。例如在CTLA-4抗体,伊匹单抗基础上增加纳武单抗[24]。PD-1联合靶向TGF-β也可作为选择方案[25]。
免疫检查点抑制剂联合化疗(加贝伐珠单抗)治疗中或治疗后疾病进展
在免疫检查点抑制剂联合双药化疗(加贝伐珠单抗)治疗后,采用标准的二线单药化疗方案:多西他赛或者培美曲塞(非鳞NSCLC,且一线治疗中没有使用过)也许是合理的选择。化疗也具备免疫原性并有利于后续的免疫检查点抑制剂治疗[26]。在双药化疗后的二线治疗中,雷莫芦单抗或者尼达尼布(非鳞NSCLC)的加入可获益,尤其适用于早期复发和进展的肿瘤[27-29]。这也可能适用于免疫检查点抑制剂治疗后,甚至在化疗和纳武利尤单抗后的三线治疗[30,31]。如上所述,在免疫检查点抑制剂联合化疗(加贝伐珠单抗)后孤立或寡转移进展,局部消融治疗有用。后续的免疫治疗策略如有机会,可在临床试验中验证[32]。例如pegilodecakin(IL-10)[33],恩替诺特(HDAC抑制剂)[34],Toll样受体9激动剂,例如lefitolimod[35]、腺苷抑制剂[36,37]以及经肿瘤浸润淋巴细胞的过继细胞疗法[38]。
PD-1抑制剂联合CTLA4抑制剂治疗中或后进展
如果一线治疗联合使用PD-1抑制剂和CTLA4抑制剂,经典的双药化疗会是更优选择。其他的免疫调节剂可以进一步在前瞻性临床试验中验证。在孤立或者寡病灶进展中,上述的局部治疗可以用于评估。
必要的研究
如果一线使用双药化疗,那么在驱动基因阴性NSCLC中,二线治疗的选择上证据充足。随着免疫治疗逐渐推至一线,我们却无足够的证据来支持初次进展或复发后的处理。在一线治疗的临床试验中,必须监测二线和三线治疗,包含治疗方案、疗效、二线和三线的无进展生存期,这样此时上述问题才能得以解决。对一线接受免疫治疗的患者进行前瞻性登记随访也有帮助。尽管如此,通过设计临床试验来验证多线治疗后的最佳策略仍是必要的。
结论
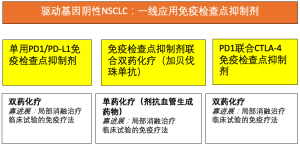
随着免疫治疗在驱动基因阴性NSCLC中逐渐推入一线,亟需复发进展后的治疗方案。而目前只有专家的共识推荐可供参考。我们的推荐见图1。根据一线治疗方案,二线治疗多数为化疗:双药化疗,如果一线方案仅为免疫治疗,一线方案为免疫治疗联合双药化疗(加贝伐珠单抗)或免疫治疗联合放化疗,二线u西安则静丹单药化疗。如果早期出现进展/复发发生较早,加抗血管生成药物(尼达尼布,雷莫芦单抗)可能提高疗效。若为孤立病灶或寡病灶进展,局部消融治疗已足够,且增强了免疫检查点抑制剂疗效。免疫治疗进一步的组合通常可在临床试验中应用。总之,我们亟需前瞻性的数据解答以上问题。
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editor Nir Peled for the series dedicated to the Congress on Clinical Controversies in Lung Cancer (CCLC 2018) published in Precision Cancer Medicine. The article has undergone external peer review.
Conflicts of Interest: The author has completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/pcm.2019.03.01). The series dedicated to the Congress on Clinical Controversies in Lung Cancer (CCLC 2018) was commissioned by the editorial office without any funding or sponsorship. RMH reports grants and personal fees from Astra Zeneca, and personal fees from Takeda, Merrimak, Chugai, Abbvie, Novartis, Bayer, BMS, Boehringer Ingelheim, Celgene, Pfizer, Roche, Lilly, Guardant Health, Mologen, MSD, outside the submitted work . The author has no other conflicts of interest to declare.
Ethical Statement: The author is accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Reck M, Rodríguez-Abreu D, Robinson AG, et al. Updated Analysis of KEYNOTE-024: Pembrolizumab Versus Platinum-Based Chemotherapy for Advanced Non–Small-Cell Lung Cancer With PD-L1 Tumor Proportion Score of 50% or Greater. J Clin Oncol 2019;37:537-46. [Crossref] [PubMed]
- Lopes G, Wu YL, Kudaba I, et al. Pembrolizumab (pembro) versus platinum-based chemotherapy (chemo) as first-line therapy for advanced/metastatic NSCLC with a PD-L1 tumor proportion score (TPS) ≥1%: Open-label, phase 3 KEYNOTE-042 study. J Clin Oncol 2018;36:LBA4. [Crossref]
- Gandhi L, Rodriguez-Abreu D, Gadgeel S, et al. Pembrolizumab plus Chemotherapy in Metastatic Non-Small-Cell Lung Cancer. N Engl J Med 2018;378:2078-92. [Crossref] [PubMed]
- Socinski MA, Jotte RM, Cappuzzo F, et al. Atezolizumab for First-Line Treatment of Metastatic Nonsquamous NSCLC. N Engl J Med 2018;378:2288-301. [Crossref] [PubMed]
- Socinski MA, Koynov KD, Berard H, et al. LBA65IMpower131: Progression-free survival (PFS) and overall survival (OS) analysis of a randomised phase III study of atezolizumab + carboplatin + paclitaxel or nab-paclitaxel vs carboplatin + nab-paclitaxel in 1L advanced squamous NSCLC. Ann Oncol 2018;29.
- Paz-Ares L, Luft A, Vicente D, et al. Pembrolizumab plus Chemotherapy for Squamous Non–Small-Cell Lung Cancer. N Engl J Med 2018;379:2040-51. [Crossref] [PubMed]
- Hellmann MD, Ciuleanu T-E, Pluzanski A, et al. Nivolumab plus Ipilimumab in Lung Cancer with a High Tumor Mutational Burden. N Engl J Med 2018;378:2093-104. [Crossref] [PubMed]
- Antonia SJ, Villegas A, Daniel D, et al. Durvalumab after Chemoradiotherapy in Stage III Non-Small-Cell Lung Cancer. N Engl J Med 2017;377:1919-29. [Crossref] [PubMed]
- Antonia SJ, Villegas A, Daniel D, et al. Overall Survival with Durvalumab after Chemoradiotherapy in Stage III NSCLC. N Engl J Med 2018;379:2342-50. [Crossref] [PubMed]
- Borghaei H, Paz-Ares L, Horn L, et al. Nivolumab versus Docetaxel in Advanced Nonsquamous Non-Small-Cell Lung Cancer. N Engl J Med 2015;373:1627-39. [Crossref] [PubMed]
- Brahmer J, Reckamp KL, Baas P, et al. Nivolumab versus Docetaxel in Advanced Squamous-Cell Non–Small-Cell Lung Cancer. N Engl J Med 2015;373:123-35. [Crossref] [PubMed]
- Herbst RS, Baas P, Kim DW, et al. Pembrolizumab versus docetaxel for previously treated, PD-L1-positive, advanced non-small-cell lung cancer (KEYNOTE-010): a randomised controlled trial. Lancet 2016;387:1540-50. [Crossref] [PubMed]
- Rittmeyer A, Barlesi F, Waterkamp D, et al. Atezolizumab versus docetaxel in patients with previously treated non-small-cell lung cancer (OAK): a phase 3, open-label, multicentre randomised controlled trial. Lancet 2017;389:255-65. [Crossref] [PubMed]
- Santini FC, Rizvi H, Plodkowski AJ, et al. Safety and Efficacy of Re-treating with Immunotherapy after Immune-Related Adverse Events in Patients with NSCLC. Cancer Immunol Res 2018;6:1093-9. [Crossref] [PubMed]
- Herbst RS, Monnet I, Novello S, et al. LBA63Long-term survival in patients (pts) with advanced NSCLC in the KEYNOTE-010 study overall and in pts who completed two years of pembrolizumab (pembro). Ann Oncol 2018;29.
- Gettinger SN, Wurtz A, Goldberg SB, et al. Clinical Features and Management of Acquired Resistance to PD-1 Axis Inhibitors in 26 Patients With Advanced Non-Small Cell Lung Cancer. J Thorac Oncol 2018;13:831-9. [Crossref] [PubMed]
- Gide TN, Wilmott JS, Scolyer RA, et al. Primary and Acquired Resistance to Immune Checkpoint Inhibitors in Metastatic Melanoma. Clin Cancer Res 2018;24:1260-70. [Crossref] [PubMed]
- Rodriguez-Ruiz ME, Vanpouille-Box C, Melero I, et al. Immunological Mechanisms Responsible for Radiation-Induced Abscopal Effect. Trends Immunol 2018;39:644-55. [Crossref] [PubMed]
- Abuodeh Y, Venkat P, Kim S. Systematic review of case reports on the abscopal effect. Curr Probl Cancer 2016;40:25-37. [Crossref] [PubMed]
- Golden EB, Demaria S, Schiff PB, et al. An abscopal response to radiation and ipilimumab in a patient with metastatic non-small cell lung cancer. Cancer Immunol Res 2013;1:365-72. [Crossref] [PubMed]
- Bauml J, Misk R, Ciunci C, et al. OA 17.08 - Phase II Study of Pembrolizumab for Oligometastatic Non-Small Cell Lung Cancer (NSCLC) Following Completion of Locally Ablative Therapy (LAT). J Thorac Oncol 2017;12:S1794-5. [Crossref]
- Sharma P, Hu-Lieskovan S, Wargo JA, et al. Primary, Adaptive, and Acquired Resistance to Cancer Immunotherapy. Cell 2017;168:707-23. [Crossref] [PubMed]
- Melero I, Berman DM, Aznar MA, et al. Evolving synergistic combinations of targeted immunotherapies to combat cancer. Nat Rev Cancer 2015;15:457-72. [Crossref] [PubMed]
- Twyman-Saint Victor C, Rech AJ, Maity A, et al. Radiation and dual checkpoint blockade activate non-redundant immune mechanisms in cancer. Nature 2015;520:373-7. [Crossref] [PubMed]
- Barlesi F, Isambert N, Felip E, et al. Initial results from phase 1 trial of M7824 (MSB0011359C), a bifunctional fusion protein targeting PD-L1 and TGF-β, in patients with NSCLC refractory or resistant to prior anti–PD-1/anti–PD-L1 agents. J Immunother Cancer 2017;5:86.
- Galluzzi L, Buque A, Kepp O, et al. Immunological Effects of Conventional Chemotherapy and Targeted Anticancer Agents. Cancer Cell 2015;28:690-714. [Crossref] [PubMed]
- Reck M, Kaiser R, Mellemgaard A, et al. Docetaxel plus nintedanib versus docetaxel plus placebo in patients with previously treated non-small-cell lung cancer (LUME-Lung 1): a phase 3, double-blind, randomised controlled trial. Lancet Oncol 2014;15:143-55. [Crossref] [PubMed]
- Garon EB, Ciuleanu T-E, Arrieta O, et al. Ramucirumab plus docetaxel versus placebo plus docetaxel for second-line treatment of stage IV non-small-cell lung cancer after disease progression on platinum-based therapy (REVEL): a multicentre, double-blind, randomised phase 3 trial. Lancet 2014;384:665-73. [Crossref] [PubMed]
- Reck M, Kerr KM, Grohé C, et al. Defining aggressive or early progressing nononcogene-addicted non-small-cell lung cancer: a separate disease entity? Future Oncol 2019; [Epub ahead of print]. [Crossref] [PubMed]
- Shiono A, Kaira K, Mouri A, et al. Improved efficacy of ramucirumab plus docetaxel after nivolumab failure in previously treated non-small cell lung cancer patients. Thorac Cancer 2019; [Epub ahead of print]. [Crossref] [PubMed]
- Corral J, Majem M, Rodríguez-Abreu D, et al. Efficacy of nintedanib and docetaxel in patients with advanced lung adenocarcinoma treated with first-line chemotherapy and second-line immunotherapy in the nintedanib NPU program. Clin Transl Oncol 2019; [Epub ahead of print]. [Crossref] [PubMed]
- Jenkins RW, Barbie DA, Flaherty KT. Mechanisms of resistance to immune checkpoint inhibitors. Br J Cancer 2018;118:9-16. [Crossref] [PubMed]
- Wong D, Goldman J, Gabrail NY, et al. 9PDPEGylated human IL-10 (AM0010) in combination with an anti-PD-1 in advanced NSCLC. Ann Oncol 2017;28:mdx710.
- Hellmann M, Jänne P, Opyrchal M, et al. OA05.01 Efficacy/Safety of Entinostat (ENT) and Pembrolizumab (PEMBRO) in NSCLC Patients Previously Treated with Anti-PD-(L)1 Therapy. J Thorac Oncol 2018;13:S330. [Crossref]
- Thomas M, Ponce-Aix S, Navarro A, et al. Immunotherapeutic maintenance treatment with toll-like receptor 9 agonist lefitolimod in patients with extensive-stage small-cell lung cancer: results from the exploratory, controlled, randomized, international phase II IMPULSE study. Ann Oncol 2018;29:2076-84. [Crossref] [PubMed]
- Mediavilla-Varela M, Castro J, Chiappori A, et al. A Novel Antagonist of the Immune Checkpoint Protein Adenosine A2a Receptor Restores Tumor-Infiltrating Lymphocyte Activity in the Context of the Tumor Microenvironment. Neoplasia 2017;19:530-6. [Crossref] [PubMed]
- Chiappori A, Williams CC, Creelan BC, et al. Phase I/II study of the A2AR antagonist NIR178 (PBF-509), an oral immunotherapy, in patients (pts) with advanced NSCLC. J Clin Oncol 2018;36:9089. [Crossref]
- Creelan B, Teer J, Toloza E, et al. OA05.03 Safety and Clinical Activity of Adoptive Cell Transfer Using Tumor Infiltrating Lymphocytes (TIL) Combined with Nivolumab in NSCLC. J Thorac Oncol 2018;13:S330. [Crossref]

赵欣宇
2015年毕业于中国医科大学七年制,获得临床医学学士,肿瘤学硕士(放射治疗)学位。2015年7月起于中国医科大学附属第一医院放疗科工作,现职称为讲师/主治医师,主要工作方向为胸部肿瘤放射治疗和立体定向放射治疗。同时于2018年考取于金明院士全日制定向博士,目前肿瘤学博士在读。从上学起我校采取专业课全英文教学,英语学习也是我的个人爱好,学生时期有过字幕组、环球科学科技新闻翻译等工作经验,工作后参加卫生部考试入选全球卫生后备人才库。从硕士阶段起了解到AME出版集团,陆续翻译多篇AME杂志、书籍等文献。(更新时间:2021/9/4)

戴映
安徽医科大学第一附属医院肿瘤内科
主治医师,肿瘤学博士
主攻胸部肿瘤内科治疗
2014年毕业于海德堡大学医学院
2017年德国汉堡大学UKE医院肿瘤中心访问学者
2017年入选全球卫生后备人才库
主持课题3项,参与省级课题多项,德国科学研究基金及德国癌症援助基金各1项
2013年度美国波士顿ASTRO会议及德国DEGRO会议壁报汇报
2020年新加坡世界肺癌大会壁报汇报
以第一作者发表SCI论文2篇,通讯作者发表SCI论文1篇
「学术任职」
安徽省全科医学会肿瘤内科分会青年委员
中国抗癌协会肿瘤营养专业委员会老年肿瘤营养学组委员
(更新时间:2021/9/4)
(本译文仅供学术交流,实际内容请以英文原文为准。)
Cite this article as: Huber RM. Disease progression in non-small cell lung cancer on immune-checkpoint inhibition, what are the options? Precis Cancer Med 2019;2:13.