
A challenge in emergency department: a case report of oxaliplatin-induced Kounis syndrome
Highlight box
Key findings
• A 52-year-old woman, was admitted to the Emergency room for angina and dyspnea few minutes after the administration the 4th cycle of oxaliplatin. No previous adverse reactions to oxaliplatin were experienced by the patient.
• Using electrocardiography, troponin levels, echocardiography and coronary angiography, we diagnosed the patient with Kounis syndrome. With a flow cytometry-based proliferation assay, the presence of oxaliplatin-specific proliferating B-cells was confirmed.
What is known and what is new?
• Hypersensitivity reactions to platinum-derived drugs represent a rare acute event. Kounis syndrome is a particular form of drug hypersensitivity that affects the cardiac tissue.
• Here we report an oxaliplatin-induced Kounis syndrome, with the observation of oxaliplatin-specific B cells that proliferate in response to oxaliplatin.
What is the implication, and what should change now?
• In an Emergency Medicine, physicians should pay attention to signs and symptoms of allergic reactions preceding an acute cardiac pain in order to recognize Kounis syndrome.
Introduction
The oxaliplatin, which is a platinum derivative, in association with capecitabine is one of the adjuvant chemoterapeutic regimens for patients with advanced colorectal cancer (1). The most common adverse effects comprise gastrointestinal, hematological and neurological symptoms (1). A hypersensitivity reaction to platinum-derived drugs represents a rare acute toxicity, however increased reports have been noted in patients exposed to multiple cycles of oxaliplatin treatment (2). Kounis syndrome, also known as “allergic angina” (3), is an underdiagnosed cause of acute coronary artery spasm secondary to the action of inflammatory mediators such as histamine, arachidonic acid metabolites, platelet activating factor and cytokines acting on endothelium and smooth muscle cells (4). There are three different known clinical manifestations of the syndrome: (I) the type 1 variant is the most common (72.6%) and characterized by vasospasm of normal coronary arteries with or without troponin leak, (II) the type 2 variant (22.3%) is identified by erosion or rupture of pre-existing atherosclerotic plaque leading to acute myocardial injury, (III) the type 3 variant (5.1%) is due to thrombosis upon a medicated stent (5). The mast cell degranulation is the main pathophysiological cause of this syndrome (6) mostly triggered by antibiotics and hymenoptera venom (7). Oxaliplatin-induced coronary vasospasm inducing Kounis syndrome is a rare adverse event (8) and so caution should be exercised when during its administration clinicians evaluate chest pain and the withdrawal of the treatment should be considered potentially leading to additional serious events, including sudden cardiac death (9). Different immunological mechanisms might be responsible for the onset of an adverse drug reaction. In particular, in sensitised individuals, upon drug administration, the cross linking of IgE molecules on the mast cell surface leads to the massive release of vasoactive molecules such as histamine and lipid mediators such as leukotriene and prostaglandins. Noteworthy, in allergic patients, it has been previously demonstrated the presence of allergen-specific circulating IgE positive B cells. Upon encounter with the cognate allergen, these cells might undergo cycles of proliferation and differentiate into IgE-producing plasma cells. Herein, we describe a case of a 52-year-old woman who had angina, dyspnea, tachycardia and wheezing after administration of oxaliplatin for colorectal cancer. Such a clinical condition is very rare but potentially life-threatening, and clinicians must be aware of its possible occurrence. We furthermore assessed for the first time, the presence and proliferative capacity of oxaliplatin-specific B cells in response to oxaliplatin, which helped us confirm our diagnostic. We present this case in accordance with the CARE reporting checklist (available at https://pcm.amegroups.com/article/view/10.21037/pcm-22-51/rc).
Case presentation
All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
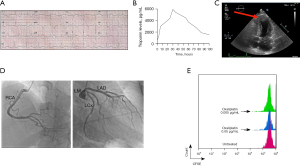
A 52-year-old never-smoker Caucasian woman, with history of allergic reaction to beta lactams (urticaria), hypertension, but no previous major cardiac events, was admitted to the Emergency room for angina and dyspnea a few minutes after the administration of oxaliplatin (the fourth cycle) as adjuvant therapy for advanced colorectal cancer. Of note, no adverse reactions were experienced by the patient in the previous oxaliplatin administrations. Upon arrival in the Emergency Department, the patient was awake, alert, and oriented, pale and referred the following symptoms: chest pain with radiation to the jaw and left shoulder with a sensation of palpitation, sense of laryngeal constriction. After acute phase medication, the patient reported a general improvement of symptoms within 2 hours. First clinical values showed hypotension (90/50 mmHg), tachycardia (105 bpm) and the oxygen saturation were 97% with a FiO2 of 21%. The electrocardiogram (Figure 1A) showed ST segment depression in DI-aVL with negative T waves and long QTc interval (560 ms); a transient ST elevation from coronary spasm was not documented. Then we evaluated the troponin (Hs-cTnI) levels over time as a readout for myocardial damage. As shown in Figure 1B, at time 0 Hs-cTnI was 577 pg/mL, reaching a peak of 5,945 pg/mL after 35 hours with subsequent steady decline. The transthoracic cardiac ultrasound (Figure 1C) highlighted hypokinesia of anterior and lateral apex, as well as of anterior and middle septal wall, with a preserved global systolic function [left ventricular ejection fraction (LVEF) 66%], suggesting a non-ST-elevation myocardial infarction (NSTEMI). The patient was treated in the Emergency Department with methylprednisolone 250 mg, chlorphenamine 10 mg, acetylsalicylic acid 200 mg, loading dose of ticagrelor (180 mg), heparin 5,000 UI and metoprolol 5 mg. The patient had resolution of the clinical symptoms about 2 hours upon admission. About 4 hours after the hospital admission, an urgent invasive coronary angiography was performed, documenting only mild luminal irregularities (Figure 1D) which is why intracoronary imaging was not performed. The patient was hospitalized in coronary care unit (CCU) and we observed a remission of both cardiac symptoms and ST depression with normalized T wave and no anomalies at cardiac ultrasound. Finally, to corroborate the hypothesis of a type I hypersensitivity reaction, we sought for the Oxaliplatin-specific B cells. Upon isolation of peripheral blood mononuclear cells, a carboxyflurescein succinimidyl ester (CFSE)-based proliferation test was performed as described before (10) with increasing doses of Oxaliplatin. Interestingly we found proliferation of B cells (CD19+) but not T cells (CD3+; data not shown) in response to the tested drug as seen by the reduction in the CFSE’s intensity when compared to untreated cells (Figure 1E). These results confirm an existing type I hypersensitivity towards oxaliplatin. Of note, this latter observation and the absence of eosinophilia on peripheral blood ruled out a possible eosinophilic myocarditis. Indeed, the most likely diagnosis was a NSTEMI due to a type 1 Kounis syndrome. The patient was finally discharged with no clinical symptoms and on adverse reactions, with indication to continue dual antiplatelet therapy with acetylsalicylic acid and clopidogrel for one month. In particular before being discharged loading dose of ticagrelor 180 mg, flectadol 200 mg, heparin 5,000 IU, metoprolol 5 mg, methylprednisone 250 mg and chlorphenamine 10 mg. The patient was subsequently discharged with acetylsalicylic acid 100 mg/day and clopidogrel 75 mg; pending the evaluation of the best oncological treatment, in view of the decision not to administer oxaliplatin yet, no calcium channel blocker was prescribed.
Discussion
In conclusion, a final diagnosis of Kounis syndrome type I variant induced by oxaliplatin has been made, based on the clinical history together with the exclusion of any other possible cause of acute coronary syndrome. Moreover, this is the first report showing a positive B cell proliferation assay in response to oxaliplatin. Of note the allergic angina is often a neglected diagnosis in the Emergency department in the case of patients with chest pain. To our knowledge, case reports have previously described pharmacological triggers of allergic angina drugs such as (I) antibiotics, e.g., cephalosporins (11) and fluoroquinolones (12) and (II) non-steroidal anti-inflammatory drugs such as ibuprofen (13) or acetaminophen (14). Kounis syndrome induced upon oxaliplatin administration is an extremely rare event according to the literature and previously described mainly as type I variant: with ST-segment elevation and normal arteries during coronary angiography (8). In our case, a final diagnosis of Kounis syndrome type I variant induced by oxaliplatin has been suspected, based on the clinical history together with the absence of any angiographic images consistent with plaque thrombosis; in fact, despite not documented, a prolonged vasospasm of one or more coronary arteries probably induced an oxygen supply reduction, resulting in an acute subendocardial ischaemia (type II myocardial infarction) (15) in the setting of an allergic response.
These observations might be useful for physicians in Emergency Department paying attention to signs and symptoms of allergic reaction preceding an acute cardiac pain in order to recognize Kounis syndrome. In an Emergency Medicine setting, the right diagnosis and the adequate treatment of this syndrome still represents a real challenge because it requires the knowledges on both drug allergy and myocardial injury. A correct diagnosis is fundamental to avoid post-allergic myocardial effects including ischemia, conduction defects, arrhythmias and dysfunction of the cardiac muscle cells.
Conclusions
In conclusion, this case report gives helpful tools to correctly diagnose Kounis syndrome in an emergency setting.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the CARE reporting checklist. Available at https://pcm.amegroups.com/article/view/10.21037/pcm-22-51/rc
Peer Review File: Available at https://pcm.amegroups.com/article/view/10.21037/pcm-22-51/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://pcm.amegroups.com/article/view/10.21037/pcm-22-51/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- National Comprehensive Cancer Network. Colon Cancer (Version 2.2017). Available online: https://www.nccn.org/professionals/physician_gls/pdf/colon.pdf. Accessed June 30, 2017.
- Thomas RR, Quinn MG, Schuler B, et al. Hypersensitivity and idiosyncratic reactions to oxaliplatin. Cancer 2003;97:2301-7. [Crossref] [PubMed]
- Kounis NG. Kounis syndrome (allergic angina and allergic myocardial infarction): a natural paradigm? Int J Cardiol 2006;110:7-14. [Crossref] [PubMed]
- Kounis NG. Coronary hypersensitivity disorder: the Kounis syndrome. Clin Ther 2013;35:563-71. [Crossref] [PubMed]
- Abdelghany M, Subedi R, Shah S, et al. Kounis syndrome: A review article on epidemiology, diagnostic findings, management and complications of allergic acute coronary syndrome. Int J Cardiol 2017;232:1-4. [Crossref] [PubMed]
- Kovanen PT, Kaartinen M, Paavonen T. Infiltrates of activated mast cells at the site of coronary atheromatous erosion or rupture in myocardial infarction. Circulation 1995;92:1084-8. [Crossref] [PubMed]
- Kounis NG, Zavras GM. Histamine-induced coronary artery spasm: the concept of allergic angina. Br J Clin Pract 1991;45:121-8. [Crossref] [PubMed]
- Chang PH, Hung MJ, Yeh KY, et al. Oxaliplatin-induced coronary vasospasm manifesting as Kounis syndrome: a case report. J Clin Oncol 2011;29:e776-8. [Crossref] [PubMed]
- Marchesini D, Esperide A, Tilli P, et al. Allergic acute coronary syndrome: a case report with a concise review. Eur Rev Med Pharmacol Sci 2020;24:11768-72. [PubMed]
- Albanesi M, Pasculli C, Giliberti L, et al. Immunological characterization of onion (Allium cepa) allergy. Postepy Dermatol Alergol 2019;36:98-103. [Crossref] [PubMed]
- Sequeira T, Gaspar Â, Mota I, et al. Kounis Syndrome Associated With Selective Anaphylaxis to Cefazolin. J Investig Allergol Clin Immunol 2018;28:257-8. [Crossref] [PubMed]
- Almeida J, Ferreira S, Malheiro J, et al. A rare cause of acute coronary syndrome: Kounis syndrome. Rev Port Cardiol 2016;35:699.e1-4. [Crossref] [PubMed]
- Akçay M. Ibuprofen-induced Kounis syndrome with diffuse ST segment depression and atrial fibrillation. Anatol J Cardiol 2017;18:380-1. [Crossref] [PubMed]
- Vu VH, Nguyen KD, Nguyen CD, et al. A Case of Kounis Syndrome Presenting as Coronary Artery Spasm Associated with Acetaminophen Infusion. Am J Case Rep 2021;22:e934190. [Crossref] [PubMed]
- Thygesen K, Alpert JS, Jaffe AS, et al. Fourth universal definition of myocardial infarction (2018). Eur Heart J 2019;40:237-69. [Crossref] [PubMed]
Cite this article as: Albanesi M, Didonna R, Chaoul N, Mazzone F, Zurlo M, Iacovelli F, Monitillo F, Rimmaudo F, Tucci M, Cives M, Porta C, Procacci V. A challenge in emergency department: a case report of oxaliplatin-induced Kounis syndrome. Precis Cancer Med 2023;6:18.

