Locally advanced HPV-positive oropharyngeal cancer cured with single agent pembrolizumab in a patient using cannabis: a case report
Highlight box
Key findings
• Pembrolizumab can be effective as a single agent in the first-line treatment of patients with locally advanced HPV-positive OPSCC.
What is known and what is new?
• Currently, ICI are primarily used in relapsed and metastatic OPSCC.
• Our case complements the limited data on the use of pembrolizumab as a single agent in treatment-naive patients with locally advanced OPSCC.
• Moreover, this study potentially extends the scarce information about cannabis use in combination with ICI.
What is the implication, and what should change now?
• Pembrolizumab should be considered as a first-line monotherapy option in treatment of locally advanced HPV-positive OPSCC, especially when patients are concerned about morbidity associated with standard CCRT.
• Risks and benefits of concurrent use of cannabis in patients treated with ICI should be carefully reviewed.
• Further studies are needed to understand the convoluted interplay between PD-L1 and HPV status in OPSCC and to evaluate the immunomodulatory effect of cannabis.
Introduction
During the last few decades, tobacco consumption in the United States has substantially decreased. It has resulted in an overall decline in the incidence of smoking-dependent oral squamous cell carcinoma (1). Nevertheless, we have been able to observe an increase in the incidence of head and neck squamous cell carcinomas (HNSCC), mostly due to an increased number of cases of oropharyngeal squamous cell carcinoma (OPSCC), which is related to human papillomavirus (HPV) infection among older adults (2,3). The current state of immune checkpoint inhibitors (ICI) use in HPV-positive HNSCC includes the following options. First-line treatment of recurrent or metastatic disease without previous systemic therapy involves pembrolizumab in combination with platinum and fluorouracil. First-line, single-agent treatment with pembrolizumab is used in patients with recurrent or metastatic HNSCC who have high programmed death-ligand 1 (PD-L1) expression (combined positive score ≥1) (4). Lastly, single-agent nivolumab or pembrolizumab can be used in patients with recurrent or metastatic disease who have failed prior platinum-based therapy (5).
ICI have not yet been approved as single agents in first-line therapy for localised or locally advanced HPV-positive OPSCC in patients who are eligible for concurrent chemoradiotherapy (CCRT) or surgery. Although initial studies of ICI have shown a direct correlation between PD-L1 expression and objective response, numerous subsequent studies showed substantial benefit from ICI irrespective of PD-L1 status (6-8). There is limited data about the use of pembrolizumab as a single first-line agent in locally advanced HPV-positive OPSCC. To the authors’ awareness, there are no publications that address this type of use. The present case report aims to describe the features and outcomes of a patient who was successfully treated with pembrolizumab for HPV-positive OPSCC. Data presented in this case report can inspire more comprehensive studies revealing new potential treatment implications of ICI in the treatment of OPSCC. Our case also adds to the limited literature on cannabis use in patients treated with ICI and, to our knowledge, depicts the first positive impact of prolonged cannabis use in combination with ICI. The manuscript is written following the CARE reporting checklist (available at https://pcm.amegroups.com/article/view/10.21037/pcm-22-53/rc).
Case presentation
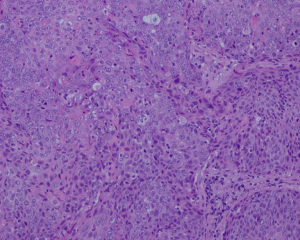
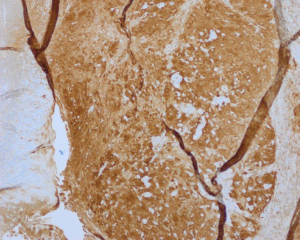
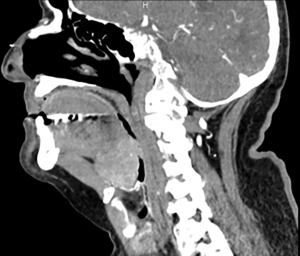
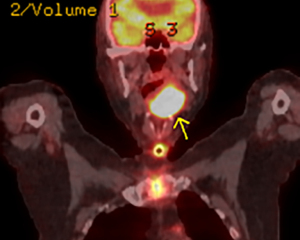
A 78-year-old man, who had quit cigarette smoking at age 45, with coronary artery disease, presented to the emergency room in February 2018 with uncontrolled epistaxis and progressive dysphagia (Figure 1). Physical exam on presentation revealed a large, nearly completely obstructing oropharyngeal mass. An emergent tracheostomy was performed and a gastrojejunal feeding tube was placed. Pathology from the base of the tongue biopsy was consistent with p16-positive moderately differentiated squamous cell carcinoma (Figures 2,3). Imaging workup was consistent with clinical tumor-node-metastasis status T3N0M0 (Figures 4,5). The patient refused treatment with CCRT, but later voiced interest in immunotherapy, as his sister, who had had lung cancer, was successfully treated with immunotherapy. PD-L1 immunohistochemistry expression was performed and showed a tumor proportion score of 90% (Figure 6). Off-label treatment with pembrolizumab at a dose of 200 mg every 21 days was started and in a year the patient achieved a complete response. Tracheostomy was reversed and the feeding tube was removed. The patient received a total of two and a half years of pembrolizumab therapy starting August 2018 and continuing until March 2021 and, as his multiple exams and scans were reassuring, pembrolizumab was discontinued in March 2021. In January 2022, he was admitted with chest pain, was diagnosed with myocardial infarction, and underwent percutaneous coronary intervention with stent placement. He was discharged 3 days later with improvement. The patient is now 83 years old. His last surveillance visits with otorhinolaryngology and medical oncology were in June 2022 and both exam and imaging revealed no evidence of disease (Figure 7). At the time of his last visit, the patient disclosed that during the first year after his diagnosis with cancer, he was using daily cannabis oil that was supplied by his family. The patient reported taking a liquid 0.3% mixture of cannabidiol and tetrahydrocannabinol oils. He recalls taking 2 drops under the tongue once a day for about 12 months after the cancer diagnosis. At the time of this writing, the patient remains in complete remission and has not developed any immune-related adverse effects. We believe that he is cured. The patient also shared his perspective with us: “I am glad I refused chemotherapy and radiation because my friends who had it did not tolerate it. Also, I would have had to remove all my teeth and I was able to save them because I refused radiation. I am glad I received immunotherapy. I think marijuana helped my treatment and helped me to get through it”.

All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Discussion
Despite the fact that the incidence of HNSCC has decreased owing to decreased exposure to cigarettes, the incidence of HPV-positive OPSCC has been rising (9). HPV-positive OPSCC accounts for more than two-thirds of all OPSCC cases in the United States (10). HPV-positive OPSCC is more prevalent among Caucasian males and is associated with a higher overall survival rate and a reduced recurrence rate following conventional therapy (11,12). The rate of tobacco use is significantly lower among patients with HPV-positive OPSCCs than their HPV-negative counterparts (13).
ICI have now been extensively authorised by the United States Food and Drug Administration (FDA) for a range of solid tumors and the benefit of therapy with ICI is unprecedented. We are entering a new era of surgery-free and chemoradiotherapy-free treatment for select patients with localised malignancy who are positive for biomarkers of response to ICI (14). Patients with advanced HNSCC benefit from ICI, which have improved drug tolerance and often enduring responses (15). The current standard of care for locally advanced OPSCC, CCRT, is associated with significant morbidity and long-term adverse effects influencing quality of life. Common side effects include mucositis, dysphagia, xerostomia, and dental problems. Additionally, there is an increased risk of death by suicide among head and neck cancer survivors (16).
The value of PD-L1 expression as a prognostic biomarker in a number of malignancies has been hotly contested by physicians; however, it has been FDA-approved as a reliable biomarker in several malignancies for a selection of patients for ICI therapy. The predictive potential of PD-L1 expression in HNSCC is not completely understood, and the immune landscape of HPV-positive versus HPV-negative tumors may influence cancer’s response to immunotherapy even more strongly (15,17). Additionally, there is a multifaceted interplay between tumor, host, and environmental and immunological processes that affect responsiveness, or lack thereof, to ICI (18).
As to the host and the environmental factors, one important consideration is the use of medical cannabis, which has been extensively legalised throughout the states. Cannabis derivatives have multiple positive effects and are widely used by patients with cancer for symptom management. On the other hand, currently available retrospective and observational data suggest a negative impact of cannabis on the outcomes of cancer patients treated with ICI therapy. The exact mechanism for this effect is unclear, though it may potentially be explained by the anti-inflammatory activity of cannabinoids and as a result a decreased response to ICI (19,20). At the same time, patients who use cannabis have decreased incidence of immune-related adverse events (19).
The strength of this manuscript is that it reports a unique case of a cure achieved by simultaneous use of ICI and cannabis in an elderly patient with HPV-positive OPSCC, who refused conventional therapy with CCRT. This case may provide important insights for clinicians and researchers studying the use of ICI in treatment of HPV-positive OPSCC. As CCRT pertains to several weeks of daily treatment with a high risk of morbidity, clinicians may consider use of ICI instead of CCRT in older patients with limited social support or those who are refusing conventional first-line CCRT. Additionally, the case adds to the limited literature on the impact of cannabis in patients treated with ICI and underscores the importance of further assessment of the immunomodulatory effect of cannabis and its clinical implications. Our case also highlights the role of convoluted interplay between PD-L1 and HPV status in OPSCC.
As this is a case report, it describes the treatment and outcome of a single patient and this is the main limitation of our study. Therefore the findings may not be generalizable to all patients with HPV-positive OPSCC. Additionally, the use of cannabis oil during treatment with pembrolizumab raises the possibility that the cannabis oil may have influenced the patient’s response to treatment. Further investigations are needed to evaluate the effectiveness of ICI as single agents for the treatment of locally advanced HPV-positive OPSCC in a larger patient population. If future research supports the use of ICI as single agents for the treatment of this type of cancer, it could potentially change current treatment guidelines and improve outcomes of patients. Additional research would also be necessary to evaluate the potential benefits and risks of combining cannabis with ICI in treatment of patients with cancer. Until more evidence is available, it is important for clinicians to follow current treatment guidelines and consider the potential benefits and risks of any treatment decisions for their patients with locally-advanced HPV-positive OPSCC.
Conclusions
ICI, such as pembrolizumab, have single-agent activity in locally advanced HPV-positive OPSCC and may potentially substitute first-line concurrent chemotherapy and radiation in selected patients. Combining ICI with cannabis is currently an area of controversy and further assessment of the immunomodulatory effect of cannabis is warranted.
Acknowledgments
We thank Dr. Heidi Jess for providing high quality photos of pathology slides. We also thank George Amatuni for language editing assistance.
Funding: None.
Footnote
Reporting Checklist: The authors have completed the CARE reporting checklist. Available at https://pcm.amegroups.com/article/view/10.21037/pcm-22-53/rc
Peer Review File: Available at https://pcm.amegroups.com/article/view/10.21037/pcm-22-53/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://pcm.amegroups.com/article/view/10.21037/pcm-22-53/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Mourad M, Jetmore T, Jategaonkar AA, et al. Epidemiological Trends of Head and Neck Cancer in the United States: A SEER Population Study. J Oral Maxillofac Surg 2017;75:2562-72. [Crossref] [PubMed]
- Osazuwa-Peters N, Simpson MC, Massa ST, et al. 40-year incidence trends for oropharyngeal squamous cell carcinoma in the United States. Oral Oncol 2017;74:90-7. [Crossref] [PubMed]
- Lu DJ, Luu M, Mita A, et al. Human papillomavirus-associated oropharyngeal cancer among patients aged 70 and older: Dramatically increased prevalence and clinical implications. Eur J Cancer 2018;103:195-204. [Crossref] [PubMed]
- Burtness B, Rischin D, Greil R, et al. Pembrolizumab Alone or With Chemotherapy for Recurrent/Metastatic Head and Neck Squamous Cell Carcinoma in KEYNOTE-048: Subgroup Analysis by Programmed Death Ligand-1 Combined Positive Score. J Clin Oncol 2022;40:2321-32. [Crossref] [PubMed]
- Cohen EEW, Soulières D, Le Tourneau C, et al. Pembrolizumab versus methotrexate, docetaxel, or cetuximab for recurrent or metastatic head-and-neck squamous cell carcinoma (KEYNOTE-040): a randomised, open-label, phase 3 study. Lancet 2019;393:156-67. Erratum in: Lancet 2019;393:132. [Crossref] [PubMed]
- Topalian SL, Hodi FS, Brahmer JR, et al. Safety, activity, and immune correlates of anti-PD-1 antibody in cancer. N Engl J Med 2012;366:2443-54. [Crossref] [PubMed]
- Wang X, Teng F, Kong L, et al. PD-L1 expression in human cancers and its association with clinical outcomes. Onco Targets Ther 2016;9:5023-39. [Crossref] [PubMed]
- Hamid O, Robert C, Daud A, et al. Five-year survival outcomes for patients with advanced melanoma treated with pembrolizumab in KEYNOTE-001. Ann Oncol 2019;30:582-8. [Crossref] [PubMed]
- Windon MJ, D’Souza G, Rettig EM, et al. Increasing prevalence of human papillomavirus-positive oropharyngeal cancers among older adults. Cancer 2018;124:2993-9. [Crossref] [PubMed]
- Lechner M, Liu J, Masterson L, et al. HPV-associated oropharyngeal cancer: epidemiology, molecular biology and clinical management. Nat Rev Clin Oncol 2022;19:306-27. [Crossref] [PubMed]
- Chaturvedi AK, Zumsteg ZS. A snapshot of the evolving epidemiology of oropharynx cancers. Cancer 2018;124:2893-6. [Crossref] [PubMed]
- Mahal BA, Catalano PJ, Haddad RI, et al. Incidence and Demographic Burden of HPV-Associated Oropharyngeal Head and Neck Cancers in the United States. Cancer Epidemiol Biomarkers Prev 2019;28:1660-7. [Crossref] [PubMed]
- Crotty TJ, Keane E, Cousins G, et al. Sexual Behaviour and Human Papillomavirus-Positive Oral Cavity and Oropharyngeal Cancer: An Irish Perspective. Cureus 2020;12:e11410. [Crossref] [PubMed]
- Cercek A, Lumish M, Sinopoli J, et al. PD-1 Blockade in Mismatch Repair-Deficient, Locally Advanced Rectal Cancer. N Engl J Med 2022;386:2363-76. [Crossref] [PubMed]
- Qiao XW, Jiang J, Pang X, et al. The Evolving Landscape of PD-1/PD-L1 Pathway in Head and Neck Cancer. Front Immunol 2020;11:1721. [Crossref] [PubMed]
- Osazuwa-Peters N, Simpson MC, Zhao L, et al. Suicide risk among cancer survivors: Head and neck versus other cancers. Cancer 2018;124:4072-9. [Crossref] [PubMed]
- Balermpas P, Rödel F, Krause M, et al. The PD-1/PD-L1 axis and human papilloma virus in patients with head and neck cancer after adjuvant chemoradiotherapy: A multicentre study of the German Cancer Consortium Radiation Oncology Group (DKTK-ROG). Int J Cancer 2017;141:594-603. [Crossref] [PubMed]
- Bindal P, Gray JE, Boyle TA, et al. Biomarkers of therapeutic response with immune checkpoint inhibitors. Ann Transl Med 2021;9:1040. [Crossref] [PubMed]
- Bar-Sela G, Cohen I, Campisi-Pinto S, et al. Cannabis Consumption Used by Cancer Patients during Immunotherapy Correlates with Poor Clinical Outcome. Cancers (Basel) 2020;12:2447. [Crossref] [PubMed]
- Biedny A, Szpunar S, Abdalla A, et al. The effect of concomitant cannabinoids during immune checkpoint inhibitor treatment of advanced stage malignancy. J Clin Oncol 2020;38:abstr e15064.
Cite this article as: Abdyraimov A, Karpovich N, Tkachuk L, Darbinyan K. Locally advanced HPV-positive oropharyngeal cancer cured with single agent pembrolizumab in a patient using cannabis: a case report. Precis Cancer Med 2023;6:19.